
 Data Structure
Data Structure Networking
Networking RDBMS
RDBMS Operating System
Operating System Java
Java MS Excel
MS Excel iOS
iOS HTML
HTML CSS
CSS Android
Android Python
Python C Programming
C Programming C++
C++ C#
C# MongoDB
MongoDB MySQL
MySQL Javascript
Javascript PHP
PHP
- Selected Reading
- UPSC IAS Exams Notes
- Developer's Best Practices
- Questions and Answers
- Effective Resume Writing
- HR Interview Questions
- Computer Glossary
- Who is Who
Acute Hemolytic Transfusion Reaction (AHTR): Signs, Symptoms, Diagnosis, and Treatment
Introduction
Acute Hemolytic Transfusion Reaction (AHTR) is a serious and potentially life-threatening complication that can occur during a blood transfusion. AHTR occurs when the recipient's immune system recognizes the transfused red blood cells as foreign and attacks them, causing the cells to break down and release their contents into the bloodstream.
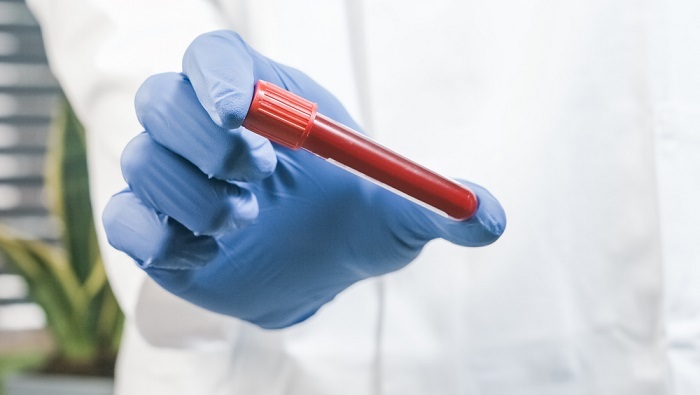
AHTR can be prevented by proper blood typing and cross-matching before transfusion, and prompt recognition and management of symptoms if they occur.
AHTR is uncommon, but it can have serious consequences, including renal failure, disseminated intravascular coagulation (DIC), and death.
Signs and Symptoms
AHTR can occur within minutes to hours after the start of transfusion. The symptoms may vary depending on the severity of the reaction, but some of the most common ones include fever, chills, back pain, chest pain, shortness of breath, rapid heartbeat, and low blood pressure. The patient may also experience hemoglobinuria, which is the presence of hemoglobin in the urine, resulting in a reddish or brownish color.
In severe cases, the patient may develop DIC, which is a condition characterized by abnormal clotting and bleeding. DIC can lead to organ failure and even death. Other symptoms of AHTR may include nausea, vomiting, headache, and confusion.
The signs and symptoms of Acute Hemolytic Transfusion Reaction (AHTR) can vary from mild to severe and may include ?
Fever and chills.
Nausea and vomiting.
Back pain and chest pain.
Shortness of breath.
Rapid heart rate.
Low blood pressure.
Dark urine.
Jaundice (yellowing of the skin and eyes).
Anxiety or restlessness.
Headache.
If left untreated, AHTR can cause severe complications such as kidney failure, shock, and even death. Therefore, it is important to seek immediate medical attention if any of the above symptoms occur during or after a blood transfusion.
Diagnosis
AHTR can be challenging to diagnose because its symptoms may overlap with other conditions. However, a healthcare provider may suspect AHTR if the patient experiences symptoms during or shortly after the transfusion.
The diagnosis can be confirmed by laboratory tests that show evidence of hemolysis, such as a low hemoglobin level, elevated lactate dehydrogenase (LDH) level, and decreased haptoglobin level. A direct antiglobulin test (DAT) can also be performed to detect the presence of antibodies on the surface of the patient's red blood cells.
The exact diagnosis of Acute Hemolytic Transfusion Reaction (AHTR) is typically based on the symptoms that the patient presents with and confirmed by laboratory tests. If patient experiences symptoms that are consistent with AHTR during or after a blood transfusion, the healthcare provider will typically order laboratory tests to confirm the diagnosis.
The laboratory tests may include a complete blood count (CBC), coagulation studies, liver function tests, and kidney function tests. The tests may also include a direct antiglobulin test (DAT) to detect antibodies that are attached to red blood cells, and a crossmatch test to determine if there is a mismatch between the donor and recipient blood types.
If the laboratory tests confirm the diagnosis of AHTR, immediate treatment will be initiated to manage the symptoms and prevent complications. The treatment may include stopping the transfusion, administering medications to manage symptoms such as pain and fever, and providing supportive care such as fluids and oxygen therapy.
Treatment
The treatment of AHTR depends on the severity of the reaction. In mild cases, the transfusion can be stopped, and the patient may receive medications to manage their symptoms, such as acetaminophen for fever and painkillers for back pain. In more severe cases, the patient may require hospitalization and intensive care.
The primary goal of treatment is to prevent further hemolysis and manage the patient's symptoms. The healthcare provider may prescribe corticosteroids, such as prednisone, to suppress the patient's immune system and reduce the risk of further hemolysis.
The patient may also receive intravenous fluids and blood products, such as albumin and fresh frozen plasma, to support their blood pressure and clotting factors.
If the patient develops DIC, they may require additional interventions, such as anticoagulation therapy or transfusions of platelets or clotting factors. In severe cases of DIC, the patient may require mechanical ventilation, dialysis, or even surgery.
Prevention
AHTR can be prevented by ensuring that the blood transfusion is compatible with the patient's blood type and by following proper transfusion protocols. The healthcare provider should perform a crossmatch test before administering the transfusion to ensure that the donor's blood is compatible with the patient's blood. They should also monitor the patient closely during the transfusion and be prepared to respond quickly if the patient develops symptoms.
Conclusion
AHTR is a severe and potentially life-threatening complication of blood transfusions. It can occur within minutes to hours after the start of transfusion and can lead to renal failure, DIC, and death. The diagnosis can be confirmed by laboratory tests that show evidence of hemolysis, and the treatment depends on the severity of the reaction.
To prevent AHTR, proper transfusion protocols should be followed, including performing a crossmatch test before administering the transfusion and closely monitoring the patient during the transfusion. If AHTR is suspected, prompt recognition and management can improve the patient's outcomes.

