
 Data Structure
Data Structure Networking
Networking RDBMS
RDBMS Operating System
Operating System Java
Java MS Excel
MS Excel iOS
iOS HTML
HTML CSS
CSS Android
Android Python
Python C Programming
C Programming C++
C++ C#
C# MongoDB
MongoDB MySQL
MySQL Javascript
Javascript PHP
PHP
- Selected Reading
- UPSC IAS Exams Notes
- Developer's Best Practices
- Questions and Answers
- Effective Resume Writing
- HR Interview Questions
- Computer Glossary
- Who is Who
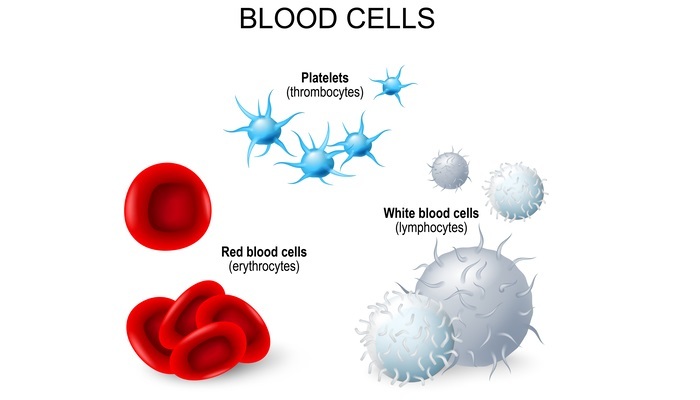
Platelets and Their Role in Clotting
Introduction
Platelets, also known as thrombocytes, are small, colourless, disc-shaped cells that play a crucial role in haemostasis, a process by which bleeding is stopped in injured blood vessels. Platelets are produced in the bone marrow and circulate in the blood until they are needed to form a blood clot. The clotting process involves a complex interplay between platelets, coagulation factors, and blood vessel walls.
Platelet Structure and Function
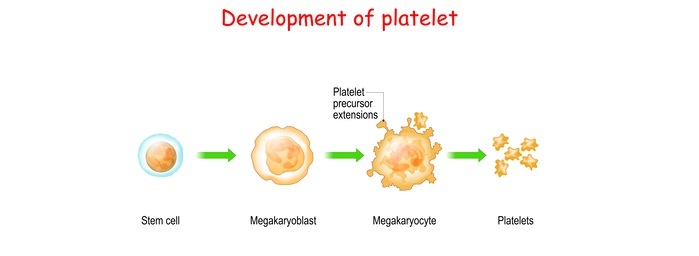
Platelets are the smallest of the three types of blood cells, with an average size of 2-3 µm in diameter. They are produced by megakaryocytes in the bone marrow, which release fragments of their cytoplasm into the bloodstream.
These fragments, called platelets, are then capable of moving through the bloodstream and responding to signals from injured blood vessels. Platelets are not true cells, but rather small packets of cytoplasm that contain various components necessary for clotting.
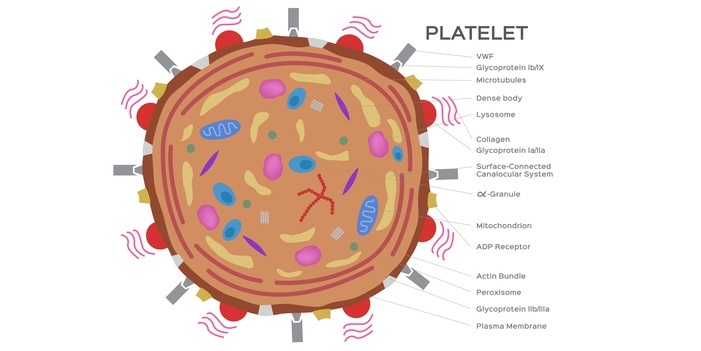
These components include granules containing platelet-derived growth factor (PDGF), serotonin, and histamine, which are released upon activation and help to recruit other platelets to the site of injury.
Additionally, platelets contain a variety of enzymes and clotting factors, including thromboxane A2 and ADP, which contribute to the formation of a clot. Platelets are activated by a variety of signals, including collagen exposed by damaged blood vessel walls, thrombin produced by the coagulation cascade, and various cytokines and chemokines released by other platelets and injured tissues.
Upon activation, platelets undergo a process called shape change, in which they transform from their resting discoid shape to a more spherical form with numerous pseudopodia.
This shape change is necessary for platelets to adhere to each other and to the exposed collagen in the injured blood vessel wall.
Once adhered, platelets undergo a process called aggregation, in which they bind to each other and form a plug that occludes the site of injury. This process is mediated by the glycoprotein IIb/IIIa receptor on the surface of platelets, which binds to fibrinogen and other adhesive proteins. The resulting platelet plug serves to prevent further blood loss from the injured vessel.
Platelet Activation
Platelet activation is a complex process that involves multiple signalling pathways and numerous platelet receptors.
Some of the key signalling pathways involved in platelet activation include the protein kinase C (PKC) pathway, the phospholipase C (PLC) pathway, and the cyclic AMP (cAMP) pathway.
The PKC pathway is activated by a variety of signals, including collagen, thrombin, and various cytokines and chemokines.
Upon activation, PKC activates a number of downstream effectors, including the PLC pathway, which is responsible for the production of inositol triphosphate (IP3) and diacylglycerol (DAG).
These second messengers help to increase the intracellular calcium concentration, which is necessary for platelet activation and aggregation.
The cAMP pathway, on the other hand, is inhibitory to platelet activation. This pathway is activated by prostacyclin (PGI2), a molecule produced by the endothelial cells lining the blood vessels. PGI2 activates the G protein-coupled receptor (GPCR) on the surface of platelets, which leads to the production of cAMP by adenylate cyclase.
cAMP inhibits platelet activation by decreasing the intracellular calcium concentration and inhibiting the activation of the PKC and PLC pathways.
Aspirin and Platelet Function
Aspirin is a commonly used medication that is known to inhibit platelet function. Aspirin irreversibly inhibits the cyclooxygenase (COX) enzyme, which is responsible for the production of thromboxane A2, a molecule that promotes platelet activation and aggregation. By inhibiting thromboxane A2 production, aspirin prevents platelet aggregation and can reduce the risk of blood clots.
Conclusion
Platelets are small but powerful cells that play a crucial role in the clotting process. Through a complex interplay of signalling pathways and receptors, platelets are able to respond to injury and form a plug that prevents further blood loss from the injured vessel.
However, platelet disorders can lead to either excessive bleeding or excessive clotting, highlighting the importance of proper platelet function.
By understanding the role of platelets in clotting and the medical conditions associated with platelet dysfunction, we can better appreciate the importance of these tiny but mighty cells in maintaining our health and well-being.
FAQs
Q1. What are platelets and what is their role in clotting?
Ans. Platelets are small, disk-shaped cells that circulate in the blood and play a crucial role in the clotting process. When a blood vessel is injured, platelets are activated and begin to form a plug at the site of injury, preventing further blood loss.
Q2. Can platelet disorders lead to both excessive bleeding and excessive clotting?
Ans. Yes, platelet disorders can lead to either excessive bleeding or excessive clotting, depending on the nature of the disorder. For example, thrombocytopenia (low platelet count) can lead to excessive bleeding, while thrombocytosis (high platelet count) can lead to excessive clotting.
Q3. What is von Willebrand disease and how does it affect platelet function?
Ans. Von Willebrand disease is a genetic disorder characterized by a deficiency or dysfunction of von Willebrand factor (vWF), a protein that plays a crucial role in platelet function and coagulation.
vWF is responsible for mediating the initial adhesion of platelets to the injured blood vessel wall, as well as serving as a carrier protein for factor VIII, a clotting factor that is essential for the formation of a stable blood clot.
Patients with von Willebrand disease may experience excessive bleeding, as their platelets are unable to form a stable clot in response to injury.
Q4. Can platelet function be measured clinically?
Ans. Yes, platelet function can be measured using a variety of tests, including the bleeding time test, platelet aggregation test, and platelet function analyzer (PFA) test.
Q5. What is Glanzmann's thrombasthenia and how does it affect platelet function?
Ans. Glanzmann's thrombasthenia is a rare genetic disorder characterized by a deficiency or dysfunction of the glycoprotein IIb/IIIa receptor on the surface of platelets. This receptor is responsible for mediating platelet aggregation, and patients with Glanzmann's thrombasthenia may experience excessive bleeding due to an inability to form a platelet plug in response to injury.
Q6. Can platelets be used in medical treatments?
Ans. Yes, platelets can be used in a variety of medical treatments, including transfusions for patients with low platelet counts and platelet-rich plasma (PRP) therapy for musculoskeletal injuries and other conditions. Platelet-derived growth factors can also be used to promote tissue healing and regeneration.

